Applications / coatings on orthopedic implants
Thickness measurement of coatings on orthopedic implants
Orthopedic implants like hip and knee replacements are often coated using Vacuum Plasma Spraying (VPS) to solve a fundamental biological challenge: metal does not naturally bond with living bone. By using a high-temperature plasma torch to propel molten titanium or Hydroxyapatite—a mineral that makes up 70% of human bone—onto the implant, manufacturers create a highly specialized, "bio-active" surface.
This process transforms a smooth metal component into a rough, porous structure that acts like a microscopic scaffold. This topography triggers osseointegration, a process where living bone cells grow directly into the pores of the coating. By mimicking the chemical and physical properties of natural bone, plasma-coated implants eliminate the need for chemical bone cement, providing a more durable, "biological" fixation that significantly reduces the risk of the implant loosening over time.
Why it is critical to control the thickness of those Ti and HAP coatings
In this process, controlling coating thickness is critical because it dictates the mechanical integrity and biological success of the implant. If a Titanium (Ti) or Hydroxyapatite (HAP) coating is too thin, it may fail to provide enough surface area or structural "depth" for bone cells to achieve secure osseointegration, leading to premature loosening. Conversely, if the coating is too thick, it becomes prone to delamination or cracking under the stress of daily movement. Excessively thick HAP layers are particularly brittle and may resorb or flake off into the joint space, causing "third-body wear" that destroys the implant’s bearing surfaces.
Non-destructive and non-contact thickness measurement techniques are a must
Orthopedic implants are high-value, precision-engineered devices and health authorities growingly push for high-frequency control of those processes. For example, the FDA recommends that testing should be performed on "final sterilized devices from multiple lots". This not only makes destructive measurement techniques unfitted for the task, but it also blocks the contact techniques that bring a contamination risk on the sterilized parts. Additionally, the contact might also generate surface damage, measurement inaccuracy due to the rough nature of those surfaces while struggling with the complex and curved geometries of such parts.
On the other hand, 3D profilometry techniques, while non-contact and non-destructive, only capture the “outer skin” of the coated part and require a prior capture of the uncoated implant. This double measurement operation (before/after coating) multiplies the measurement uncertainties while requiring extremely precise re-positioning alignment, almost impossible to perform regarding the part complexity in geometry, roughness in surface, thermal expansion and environmental dependency.
Why laser photothermal radiometry is the perfect solution for coated implants
“ [Enovasense technology] allows us to obtain precise and reliable measurements, two attributes that are impossible to combine with conventional techniques. ”
HTI Technologies
DeviceMed Magazine, Feb 2022
Laser photothermal radiometry is the ideal technology for orthopedic coatings because it resolves the conflict between maintaining sterile integrity and ensuring precise characterization of porous surfaces. This non-contact method allows for 100% inspection of final sterilized devices. Because it uses thermal diffusion to measure thickness, it is unaffected by the "bumpy" topography of plasma-sprayed surfaces that often cause mechanical contact probes to sit only on the highest peaks. It provides a direct, absolute measurement of coating thickness in a single 1-second step, entirely bypassing the need for a "before and after" comparison. The system analyzes the internal thermal response decay of the coating, which is physically governed by the layer's depth, the thickness is thus calculated instantly from the coated part alone, ensuring 100% inspection without the errors of manual alignment or baseline subtraction.
| Criteria | Enovasense laser photothermal | Eddy currents or magnetic induction | Differential 3D profilometry |
|---|---|---|---|
| Contact | Non-contact | Contact | Non-contact |
| Implant sterility maintenance | High | No (contact needed) | Hard (Multiple manipulations required) |
| Available on Ti and HAP coatings | Yes | Only on HAP coatings | Yes |
| Impact of the high surface roughness | No impact | The contact relies on the highest peaks and overestimates the average thickness | Shadowing effect |
| Impact of complex geometries | No impact | Impacted by curved shapes and proximity to edges | Complexifies the realignment operations |
| Measurement time | Fast (1 second per point) | Fast (1 second per point) | Slow (multiple alignment, measurement and analysis steps) |
| In-situ implementation / Automation | Simple | Difficult (contact needed) | Impossible |
| 100% inspection ability | Realistic | Impossible | Impossible |
How Enovasense laser photothermal technology performs on HAP coatings
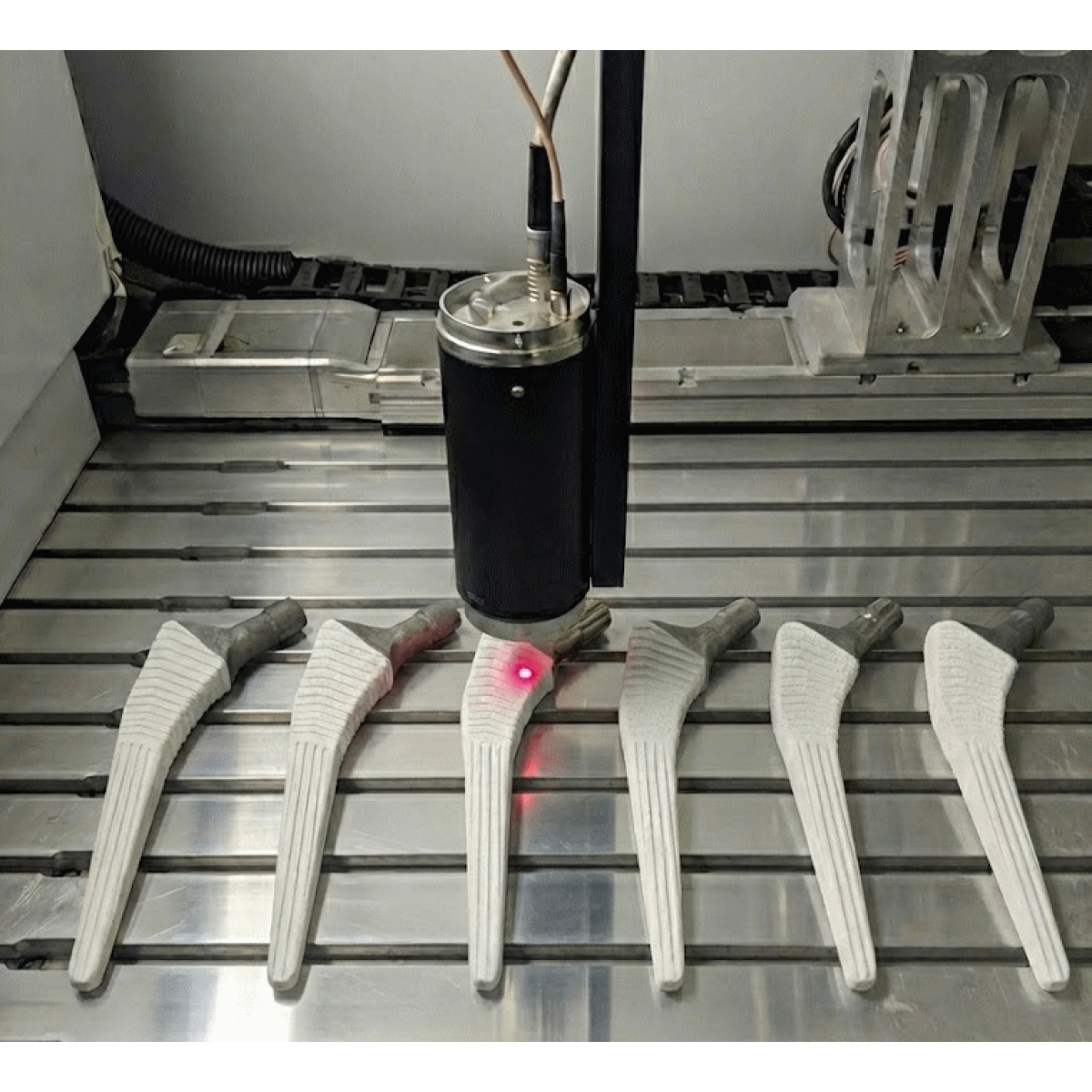
For this feasibility study, 6 titanium-based hip implants featuring HAP layer coatings of various thickness levels from 90 and 200µm.
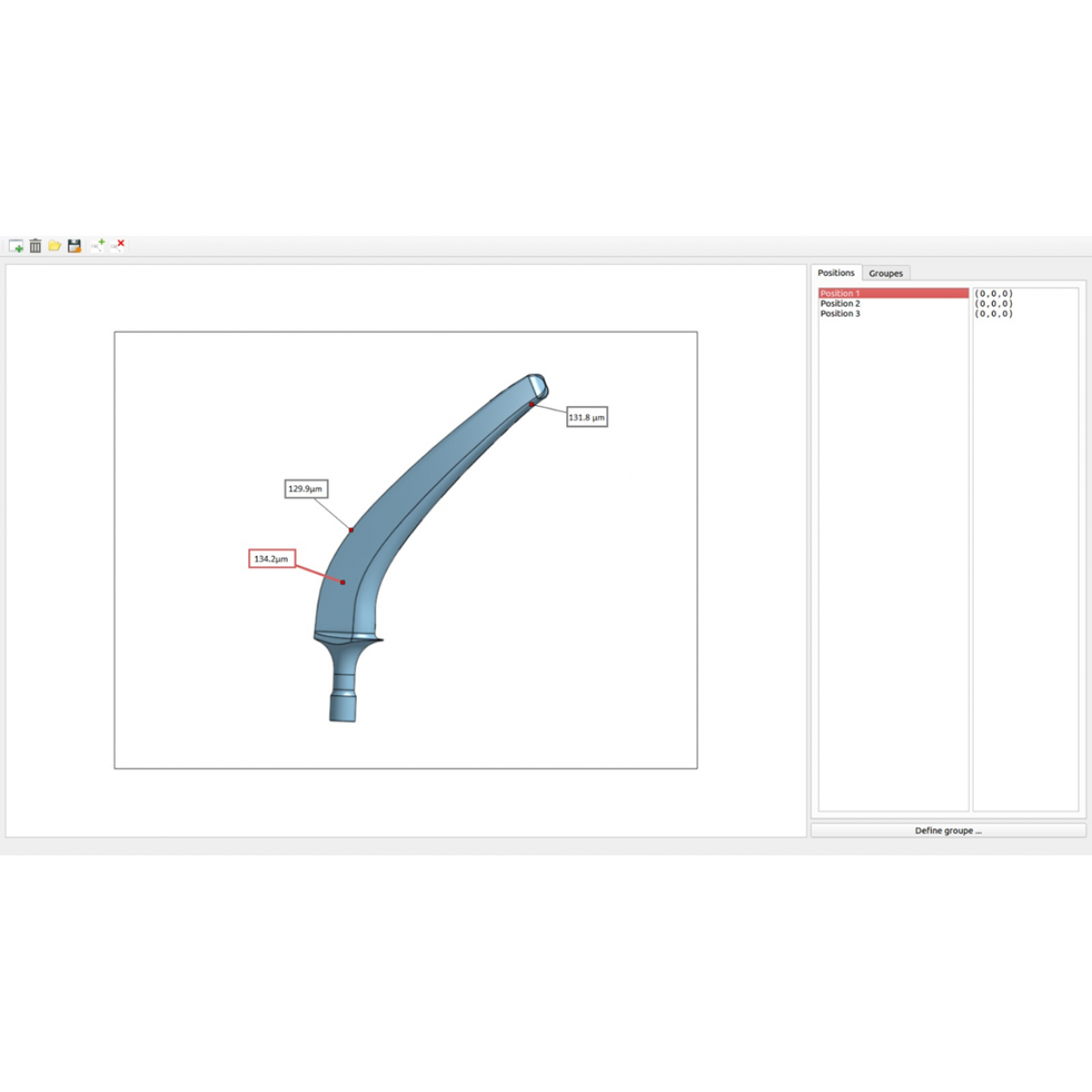
An Enovasense Point sensor was used with the following parameters : Wavelength of 980nm, laser maximum power 10W, measuring time 1s, distance probe-part 35mm and laser spot diameter of 2,6mm. The sensor was then placed into a 3 axes control station and a 2D mapping of each sample was performed with a 1 millimeter step in both directions.
The mapping is then displayed in the following figure :
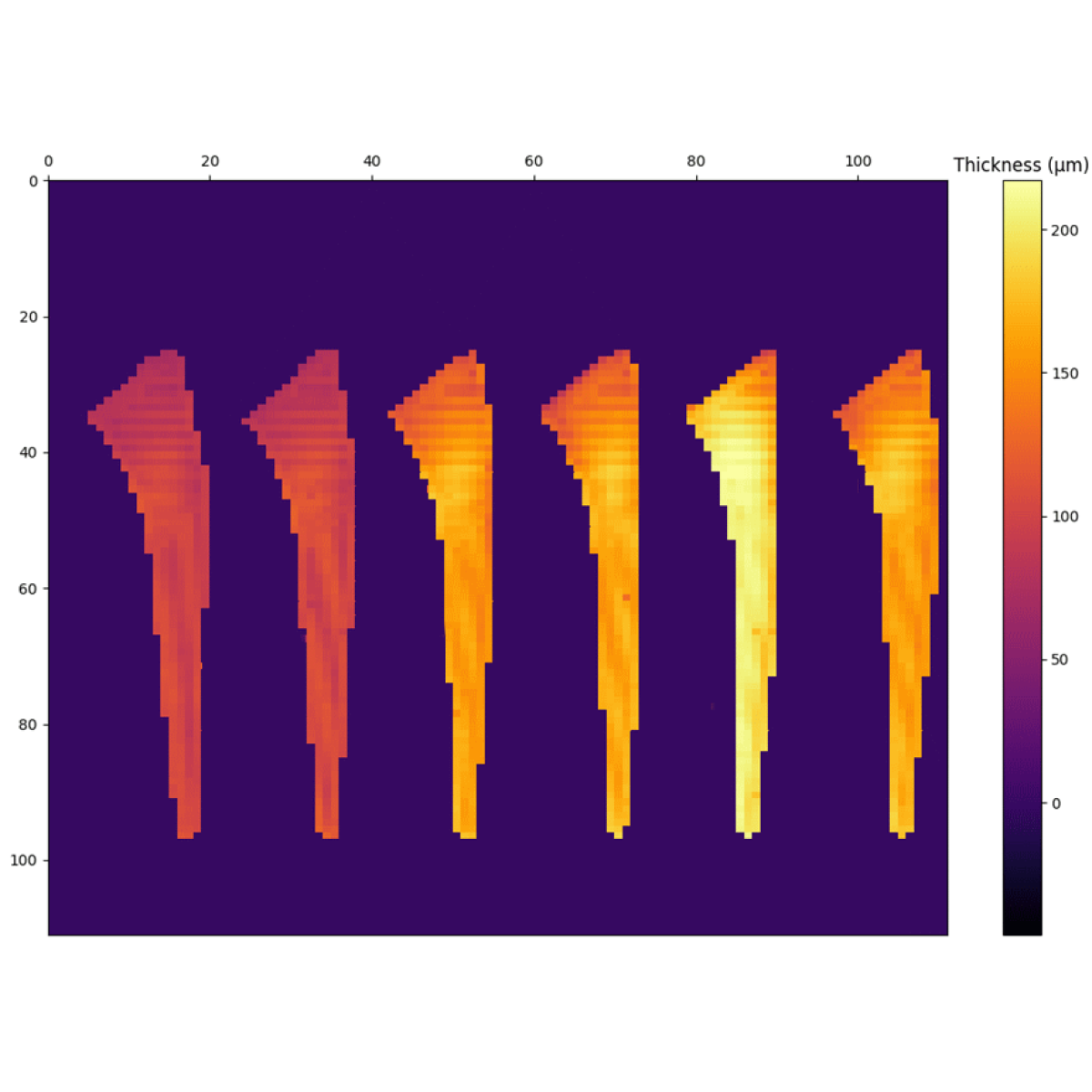
HAP coating thickness mapping on 6 hip implants (Enovasense Point sensor mapping)
The mapping shows that the laser photothermal point sensor was efficiently able to measure the coating thickness in every position of the hip implants, including in tiny areas. Those measurements are then correlated to destructive cross section microscopic measurements realized (10 positions per sample). Regarding both technologies, the average value and the standard deviations were used for the intercomparison. In the following table, the average HAP coating thickness is reported for both laser photothermal and destructive techniques. The values appear to be very close with both techniques.
| Sample | Laser photothermal average | Cross section average |
|---|---|---|
| Sample A | 96 | 94 |
| Sample B | 101 | 96 |
| Sample C | 152 | 152.6 |
| Sample D | 156 | 157.2 |
| Sample E | 193 | 185.1 |
| Sample F | 158 | 175.3 |
Intercomparison of Laser photothermal average measurements with cross section (destructive) average measurement of the HAP thickness per sample
Repeatability tests further demonstrate the high stability of this technology, with consistent results obtained across repeated measurements at identical locations.
To further assess the intrinsic performance of the measurement system, a Type 1 Measurement System Analysis (MSA) was conducted on a representative sample under controlled conditions.
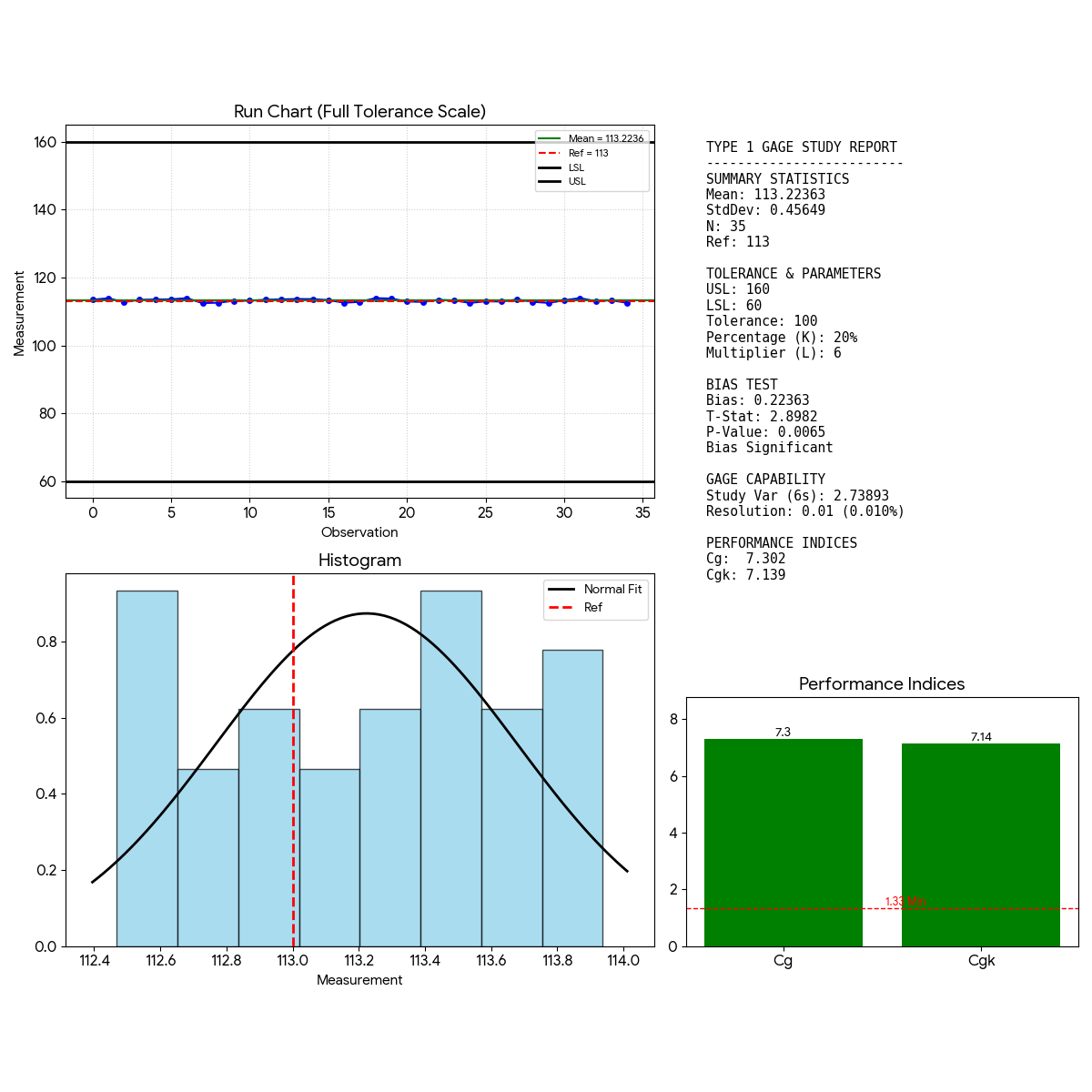
- Bias: The P-Value (0.0065) is less than 0.05, which technically means the bias is statistically significant. The average measurement (113.22) is consistently higher than the reference (113.00).
- Capability: The capability indices Cg (7.30) and Cgk (7.14) are extremely high (far above the 1.33 limit).